Multidisciplinary Treatment Model With Oncosil
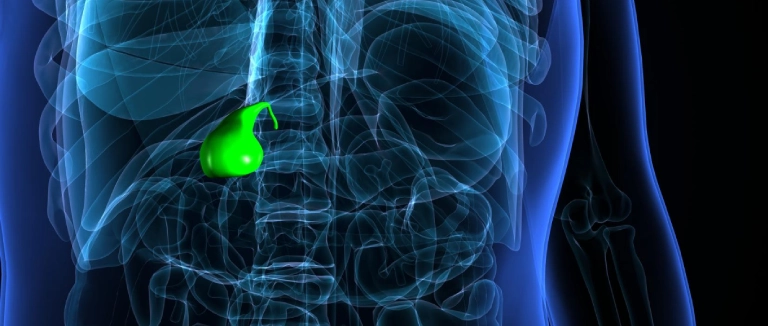
In pancreatic head cancers, Oncosil-supported multidisciplinary treatment refers to a comprehensive therapeutic approach in which, in addition to standard methods such as surgery, chemotherapy, and/or radiotherapy, Oncosil—a local radiotherapy implant containing radioactive phosphorus-32 administered intratumorally—is used.
The aim of this method is to deliver localized radiation directly targeting the tumor to reduce tumor volume, increase the likelihood of surgical resection, and enhance the effectiveness of systemic therapies.
Objective
Surgical resection remains the only potentially curative treatment for pancreatic cancer. However, in advanced stages, chemotherapy and radiotherapy have been shown to provide survival benefits.
Unfortunately, the 5-year relative survival in pancreatic cancer remains poor:
- Localized disease (confined to the pancreas): 44%
- Regional disease (spread to nearby tissues or lymph nodes): 16%
- Distant metastasis: 3%
- Overall average across all stages: ~13%
At the time of diagnosis, approximately 80% of pancreatic head cancers are unresectable. Some are classified as borderline resectable due to their close proximity or direct invasion of vital vascular structures such as the superior mesenteric vein, portal vein, or adjacent arteries. In such cases, achieving resection — especially an R0 resection (no residual tumor) — is often not feasible.
- Although neoadjuvant therapy (treatment before surgery) has not yet definitively proven to improve overall survival in borderline resectable cases, it has been shown to:
- Increase the chance of surgical resection,
- Improve R0 resection rates,
- And prolong disease-free survival.
While neoadjuvant or adjuvant therapies in pancreatic cancer are becoming more standardized, external beam radiation therapy may still cause unintended damage to surrounding tissues before reaching the tumor.
OncoSil, a radioactive phosphorus-32 (P-32) microsphere, can be injected directly into the tumor via endoscopic ultrasound (EUS) or during surgery. This technique delivers localized radiotherapy with minimal exposure to adjacent healthy tissues.
- Half-life of P-32: 14.27 days
- 98% of the radiation is absorbed by the tissue within 81 days
By integrating OncoSil-based internal radiotherapy with systemic chemotherapy, our goals are:
- To prolong overall survival,
- To convert selected patients to surgical candidates,
- And to offer individualized treatment under a robust multidisciplinary framework.
Method
1. Multidisciplinary Evaluation
- Disciplines involved: Surgery, Medical Oncology, Nuclear Medicine, Interventional Radiology, Gastroenterology
- Every case will be reviewed by a dedicated tumor board.
2. OncoSil Application
- Intratumoral injection of P-32 radioactive microspheres via EUS (endoscopically; under general anesthesia) or intraoperative approach
- Primary goal: Tumor volume and activity reduction
3. Systemic Therapy
- Standard regimens such as FOLFIRINOX or nab-paclitaxel + gemcitabine, administered concurrently or sequentially
4. Surgical Reevaluation
- Minimum of 3 months of treatment before reassessment
- Re-staging with PET/CT, MRI, and tumor markers
- Patients showing favorable response may undergo curative surgery
Who is Eligible For This Treatment?
- Patients with pancreatic head adenocarcinoma
- Those with borderline resectable or unresectable (locally advanced) tumors
- Patients able to tolerate standard FOLFIRINOX chemotherapy
- Karnofsky Performance Score ≤70 (can perform self-care but not work)
- Patients not planning pregnancy during or shortly after treatment
- Age ≥18
- Also applicable in locally advanced or recurrent cases for palliative purposes
Who is not Eligible?
- Patients with distant metastases
- Tumors involving multiple regions of the pancreas
- Cases where endoscopic access to the tumor is not possible
- History of another cancer within the past 5 years
- Pregnant or breastfeeding women
- Severe comorbidities that preclude the procedure
Why Oncosil?
- Targets tumor cells while sparing surrounding healthy tissue
- May provide a survival benefit even in non-surgical cases
- Potential for synergy with chemotherapy
- Treatment decisions are personalized by a multidisciplinary team
Center Highlights
- High-level surgical expertise with background in liver transplantation and HPB surgery
- Access to interventional radiology and nuclear medicine
- Research-friendly clinical setting
- Rapid and coordinated multidisciplinary decision-making process
- Patient-centered follow-up and side effect management system
Frequently Asked Questions About Oncosil
What Are the Side Effects of Oncosil?
Following treatment, some side effects may occur due to the injection site and the procedure itself. These may include abdominal pain, fatigue, nausea, indigestion, or gastrointestinal discomfort such as reflux. These side effects are usually short-term and can be managed easily.
Can Oncosil Be Used Together With Other Treatments?
Yes, Oncosil is usually administered in combination with chemotherapy. In most cases, the Oncosil procedure is performed during the rest week between chemotherapy cycles. Its use, particularly in combination with chemotherapy regimens containing gemcitabine and nab-paclitaxel, has been found to be safe. Your doctor will determine the most appropriate approach for your treatment plan.
Is Oncosil Permanent in the Body?
Yes, Oncosil microspheres remain permanently within the tumor tissue. However, the radiation they emit decreases over time and eventually disappears completely. The residual amount of radioactivity in the body is very low and does not harm the environment or other people.
* Contents of this page is for informational purposes only. Please consult your doctor for diagnosis and treatment. The content of this page does not include information on medicinal health care at Liv Hospital .






